Adrenal fatigue describes a condition where your body struggles to produce enough cortisol.
But other conditions, like high cortisol levels, could actually be what’s causing your symptoms!
So, you visit a natural health practitioner in hopes of treating your adrenal fatigue. All your symptoms fit so well. But after testing, you don’t have the low cortisol levels commonly found in adrenal fatigue. You have elevated cortisol levels. What’s going on?
Adrenal fatigue is incredibly underdiagnosed in conventional medicine. But in alternative medicine, adrenal fatigue is one of the most popular diagnoses. I’d argue that adrenal fatigue is so popular it’s overdiagnosed by many alternative medicine practitioners.
Adrenal fatigue describes a condition where your body has low levels of cortisol. But practitioners often forget about high cortisol levels. High cortisol levels could be the hidden cause of your stress, anxiety, fatigue, and even weight gain!
If you were told that you didn’t have adrenal fatigue, you could actually have high cortisol levels. And these elevated levels of cortisol could be quietly contributing to a lot of your symptoms!
Adrenal fatigue vs adrenal energy
For the longest time, researchers described adrenal fatigue to progress through a 3-stage model. The three stages describe increasing levels of fatigue and/or severity. This three-stage model was originally developed by Dr. Hans Selye. (1)
Selye called his theory the General Adaptation Syndrome. Selye’s research was the foundational understanding of how your body responds to stress. This is the framework we use today to explain adrenal fatigue. But it’s really just a small piece of the puzzle. Selye’s model only addresses three stages. There’s far more to adrenal fatigue than just these three steps!
Selye described the body’s response to stress as a linear event – progressing from step one to step two and so on. But in reality, your stress response does not progress in a straight line. You may think you have adrenal fatigue (low cortisol levels), but what you may actually have is high cortisol levels. The symptoms of both low and high cortisol levels can be very similar!
Everyone is so focused on low cortisol levels (adrenal fatigue) that high cortisol levels are rarely considered. Before you start an adrenal fatigue treatment plan, make sure you know exactly where your cortisol levels are at. If you actually have high cortisol levels, following the treatment plan for adrenal fatigue could make your symptoms much worse!
How researchers think you respond to stress
Much of what researchers know about stress today is founded upon Dr. Selye’s research. Unfortunately, this has resulted in pigeonholing of conditions like adrenal fatigue. Adrenal fatigue is a complex, multi-system condition. It is not as simple as three steps along a continuum.
The commonly discussed adrenal fatigue model describes three stages of increasing severity. It typically looks like:
Stage I:
- Acute HPA axis activation or adrenal stress.
- High levels of cortisol
- Symptoms often include:
- Heightened levels of anxiety
- Inability to sleep
- Feeling stressed
Stage II:
- Stress maladaptation
- Cortisol dominance with low DHEA.
- This stage is often labeled as adrenal fatigue.
- Symptoms in this stage often include a combination of stage II and stage III. There are no hallmark symptoms of stage II adrenal fatigue.
Stage III:
- HPA axis down-regulation
- Low cortisol and DHEA levels.
- This stage is often labeled adrenal exhaustion.
- Symptoms often include:
- Low energy levels
- Exhaustion
- Depression
- Lack of motivation
- Low appetite
The above three steps are useful for helping explain or understand adrenal fatigue. But it is an oversimplification. In clinical practice, there are more than three stages of cortisol imbalance.
How your cortisol should behave
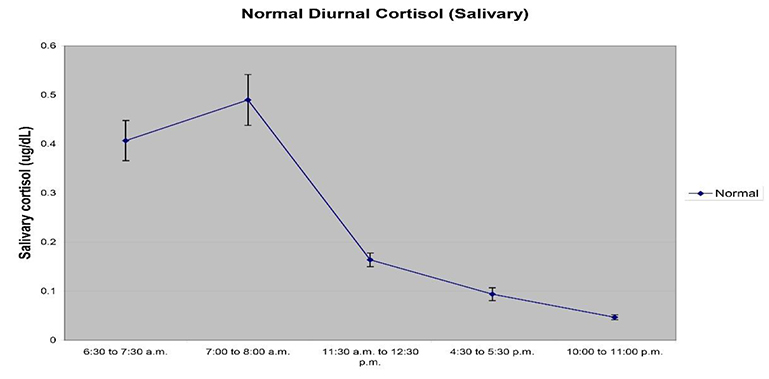
When testing for adrenal fatigue, cortisol measurements need to be taken at different points in the day. Remember, cortisol follows what is called a diurnal rhythm. Meaning its activity level is more prominent during the day.
The blood tests you do with your family doctor will not pick up slightly low or high levels of cortisol. These blood tests only pick up extreme fluctuations in your cortisol rhythm. You need to have either Cushing’s Disease (extremely high levels of cortisol) or Addison’s Disease (extremely low levels of cortisol) for conventional lab tests to pick it up.
Healthy cortisol levels
If you’re quite healthy and enjoy relatively low-stress levels, your cortisol levels will probably look something like the below graph:
 Cortisol
Cortisol
- There will be a dramatic difference between morning and evening cortisol values.
- The majority of your cortisol should drop within the first three hours after waking.
- The graph to the right illustrates a healthy cortisol rhythm.
- Each dot on the graph represents the time cortisol was measured.
- In this example, the patient woke up at 6:30 am.
- The spike in cortisol shortly after waking is called the cortisol awakening response. It should be 35-60% higher than the value at the time of waking.
- DHEA
- While not shown in this graph, morning DHEA levels should be higher than bedtime levels.
- Generally, a 50-100% difference between morning and evening DHEA levels is ideal.
This is the textbook example of healthy adrenal and cortisol function. Most people’s cortisol levels look nothing like this. If you don’t have adrenal fatigue but still feel like something’s not quite right, you could be experiencing high levels of cortisol.
Below, I’ll walk you through the most common patterns found in high levels of cortisol.
Elevated cortisol awakening response (CAR)
The cortisol awakening response (CAR) is a large surge of the cortisol hormone generally seen shortly after waking. If you look at the above graph, an elevated cortisol awakening response would show the second value on the graph near the top of the chart – or even off the chart! In this example, all other cortisol values will remain within range.
Elevated cortisol awakening response is typically indicative of high levels of anticipated daily or job stress. Some of the common symptoms associated with an elevated cortisol awakening response include: (2, 3)
- Anxiety
- Depression
- Palpitations (feeling your heartbeat)
- Sleep disturbances (waking early and being unable to fall back asleep)
The cortisol testing you do with your family doctor will not measure the cortisol awakening response. The CAR can only be measured through specific labs like DUTCH.
In the 3-stage model of adrenal fatigue, an elevation of the CAR is generally considered stage one. But remember, stress doesn’t always happen in successive stages. I’ve seen an elevated CAR combined with low levels of cortisol (adrenal fatigue) on many different occasions.
How to treat an elevated cortisol awakening response: (4)
- Identify avoidable life and/or job stressors.
- Try to regulate sleep time, duration, and quality.
- Go to bed at the same time every night.
- Ensure you’re getting 8-9 hours of sleep each night.
- Turn off lights and devices 60 minutes before bed.
- Use blackout blinds to make your room as dark as a cave.
- Support blood sugar balance through a healthy diet.
- Supplement phosphadadatyl choline
- 100-200mg 3x/day
High levels of cortisol
High levels of cortisol (hypercortisolism) occur when your cortisol levels are elevated throughout the day (at most time points) but the diurnal rhythm remains intact. (5) A healthy diurnal cortisol rhythm shows a peak in cortisol shortly after you wake up (this is the cortisol awakening response). After this cortisol surge, levels should decrease to their lowest point just before bed. While you sleep, your cortisol rises and the cycle begins again the next morning.
Cortisol levels become elevated in response to stress. (6) Remember, chronic stress usually does not relate to finances, work, or family. These contribute, no doubt. But the more insidious causes of chronic stress are blood sugar imbalance, sleep disruption, or inflammation.
How to treat high cortisol levels: (7)
- Identify and remove (if possible) the main source of stress.
- A thorough examination of blood sugar imbalances, hidden sources of inflammation, and sleep rhythm should be explored.
- Your high levels of cortisol will not improve until you’ve removed inflammation, balanced your blood sugar, and ensured you have a healthy sleep.
- Supplement phosphadadatyl choline
- 100-200mg 3x/day
- Add supplements known to lower cortisol:
- Rhodiola
- Ashwadaga
- Avoid taking licorice root or adrenal glandulars if you have elevated cortisol levels
Elevated evening cortisol
Sometimes, cortisol levels can remain in balance at all times except for the evening. When cortisol levels are elevated at the evening time point, falling asleep often becomes challenging. (8) In general, this occurs in those with ongoing, chronic inflammation. Identifying and removing the source of inflammation is paramount to success.
How to treat elevated evening cortisol: (9)
- Identify the source of inflammation:
- Undiagnosed food sensitivities/allergies and gut infections are common culprits.
- I recommend working with a knowledgeable functional medicine practitioner to help you identify exactly what could be the hidden cause of your inflammation.
- Improve your sleep hygiene
- Avoid the use of electronics before bed. If you do use electronics, ensure a blue-light blocking application is enabled.
- Consider the use of blue-light-blocking glasses.
- Relaxation or meditation techniques.
- Supplement with herbs known to promote relaxation:
- Melatonin
- Valerian root, passionflower, and skullcap are herbs commonly used to promote relaxation.
- Avoid stimulants after 12 pm.
- Caffeine
- Licorice
These are three of the most common patterns found in patients with high levels of cortisol. Remember, there are many patterns that can occur under the umbrella of adrenal fatigue. Effective treatment can only be prescribed after knowing exactly where your cortisol levels are at.
The treatment for high cortisol levels is different than the treatment for low cortisol levels. Test first. You’ll save yourself lots of time and frustration if you properly diagnose your condition first.
Now, I want to hear from you:
Do you have adrenal fatigue? Or, could high cortisol levels be the course of your symptoms?
Do you want to know more than your doctor about adrenal fatigue?

I would like to ask your explanation on some symptoms. It happened twice recently that some time after having breakfast and while standing up I felt fatigued, dizziness and cold sweat. How could that be? In the meantime I have moderate fatigue which was very light for several tears but now it is elevated and lasting.
Hi, Nikos,
What you described sounds like orthostatic hypotension. This can be associated with low levels of cortisol. More info here: https://erin-munro-clark-project.prev07.rmkr.net/is-adrenal-fatigue-syndrome-real/