How do you get diagnosed with CIRS?
Imagine waking up every day feeling like you’ve run a marathon, your body weighed down by a fatigue that you can’t sleep off. You may not even need to imagine it – this may be describing you.
As you make your way through the frustrating maze of symptoms, you may have come across a potential piece of the puzzle—Chronic Inflammatory Response Syndrome (CIRS).
Getting a diagnosis for CIRS, however, is not easy. You’ve probably learned that most doctors have never heard of CIRS, and if they have, they don’t know enough about it to make a diagnosis.
How do you get diagnosed with CIRS?
Let’s dive into the story of diagnosis, and explore the key details that may guide you toward answers.
Diagnosing CIRS: Beyond Routine Testing
For those with chronic fatigue syndrome or fibromyalgia, the journey to a CIRS diagnosis is often a long one. More and more websites touch on the basics of CIRS, but let’s take a look at the details that are often ignored.
Proper Screening:
 Routine tests run by your doctor’s office won’t pick up on the CIRS diagnostic markers. That’s why proper screening is crucial. Targeted screens, including Visual Contrast Sensitivity (VCS) testing, are key to looking for potential biotoxin exposure (Shoemaker, R. C., & House, D. E., 2006). VCS testing is also a low cost approach that indicates if more in-depth blood work is necessary.
Routine tests run by your doctor’s office won’t pick up on the CIRS diagnostic markers. That’s why proper screening is crucial. Targeted screens, including Visual Contrast Sensitivity (VCS) testing, are key to looking for potential biotoxin exposure (Shoemaker, R. C., & House, D. E., 2006). VCS testing is also a low cost approach that indicates if more in-depth blood work is necessary.
Testing the correct immune system:
Our immune system has two different subdivisions:
- The innate or nonspecific immune system
- This immune system is the first responder to any intruders (viruses, bacteria, flus etc) and it usually uses inflammation as a defence.
- The adaptive or specific immune system
- The adaptive immune system analyzes the intruder and creates a specific defence. Once it has created this defence these specific intruders will not make you sick again. It’s why once you get chicken pox you will never get it again – your immune system recognizes the virus and can immediately respond to it.
When mold enters your body your innate immune system will respond. It will then call your adaptive immune system into action to expel the toxins from your body.
However, the immune system of a CIRS patient doesn’t call their adaptive immune system into action. This leaves their innate immune system stuck fighting mold and mycotoxins on its own. The innate immune system uses inflammation to fight intruders, and it is this never-ending inflammation that is behind all of your syndromes and illnesses.
 Meet the unsung heroes of CIRS diagnosis—MMP9, C4a, TGF Beta 1, and MSH lab testing. These are biomarkers that tell us if your innate immune system is working properly. Standard blood work looks at how your adaptive immune system is working.
Meet the unsung heroes of CIRS diagnosis—MMP9, C4a, TGF Beta 1, and MSH lab testing. These are biomarkers that tell us if your innate immune system is working properly. Standard blood work looks at how your adaptive immune system is working.
Doctors often overlook these biomarkers in routine check-ups. However, they provide a much better picture of the inflammatory and innate immune response. Elevated MMP9, abnormal C4a levels, and skewed TGF Beta 1 and MSH values may signal the presence of CIRS (Shoemaker, R. C., & House, D. E., 2006).
Why traditional lab testing always misses CIRS
Conventional lab testing can not reliably detect Chronic Inflammatory Response Syndrome (CIRS) for several reasons. The main reason is because CIRS is a complex and multifaceted condition with unexpected immune responses. Here are some key factors that contribute to the challenges in conventional lab testing for CIRS:
Testing the wrong Biomarkers
CIRS involves a dysregulated immune response to biotoxins, particularly mycotoxins produced by mold. Conventional lab tests focus on general markers of inflammation, such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR). However, these markers can’t pick up the innate immune responses triggered by biotoxins.
Testing one area instead of many
CIRS appears as a wide range of symptoms that affect various systems throughout the body. However, conventional lab tests typically focus only on specific areas of concern.
CIRS has unique Biomarkers
Practitioners don’t test the biomarkers that indicate CIRS. Examples include Matrix Metallopeptidase 9 (MMP-9), Complement Component 4a (C4a), Transforming Growth Factor Beta 1 (TGF-β1), and Melanocyte Stimulating Hormone (MSH).
 Ignoring Exposure history
Ignoring Exposure history
Exposure to biotoxins triggers CIRS, especially the biotoxins from buildings with water damage. However, conventional lab tests don’t consider this. Knowing the patient’s history of environmental exposure is crucial to a CIRS diagnosis.
Every patient experience CIRS differently
CIRS is different for every patient. This is due to genetic factors, how long and how intense the biotoxin exposure was, and the patient’s overall health status. The conventional medical system prefers a one-size-fits-all approach to testing, but CIRS requires testing that is more in-depth.
Basically, CIRS is a complex condition that requires more in-depth and comprehensive testing. Standard blood work won’t cut it.
The keys to diagnosing CIRS are:
- learning about the patient’s history
- running specialized tests
This helps the practitioner identify the specific immune responses and environmental triggers that cause CIRS. This is why it is highly important for patients who think they are suffering from CIRS to find a qualified Shoemaker Protocol practitioner.
The Shoemaker Protocol is the only scientifically proven and peer reviewed method to treat CIRS. It uses a unique blood test that looks at the biomarkers specific to CIRS, and takes a patient’s history of environmental exposure into close consideration.
How do you get diagnosed with CIRS – The Shoemaker Protocol
Just like the illness, diagnosing CIRS is not easy. Patient can’t run a blood test and receive a positive or negative result. Instead, Dr. Shoemaker has a created three tiers of criteria to determine if CIRS is behind your illness.
Tier 1 Criteria
All three criteria are key:
1) Exposure
- The patient must have a history of exposure to WDB (water-damaged building), tick-borne illness, other neurotoxins (ex: Dinoflagellates, Pfiesteria, Cyanobacteria), or recluse spider bites.
2) Differential diagnosis
- Ruling out other common illnesses and other potential causes of fatigue.
- Celiac disease
- Hypothyroid
- Low iron
3) Symptoms
- Must be consistent with the peer-reviewed literature. See my post on what are the symptoms of CIRS.
- 8/13 of the CIRS-specific symptom clusters must be present.
Tier 2 Criteria
Three of the six are key:
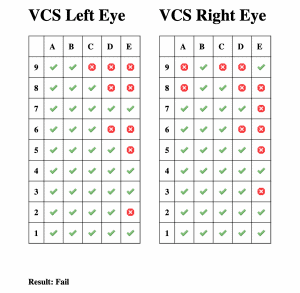
1) Abnormal VCS
- In the presence of biotoxin illness, visual contrast sensitivity decreases. Only rows C and D count for scoring pass or fail. One must see 7 in each eye on C and 6 in each eye on D. Rows C and D show improvement with the clearing of biotoxins.
2) Presence of the HLA gene
- 95% of the CIRS population will have genetic susceptibility.
3) Elevated MMP-9
- Activated by macrophages that induce inflammatory cytokines.
4) Imbalance in ACTH/Cortisol
- Both are often elevated early on in CIRS.
- As the disease progresses, low levels in both is often found.
5) ADH/Osmolality imbalance
- In CIRS patients, ADH is usually low while osmolality is usually high.
6) Low MSH
- MSH is low in 95% of patients with CIRS.
Shoemaker R. State of the Art answers to 500 Mold Questions Question 212.
Tier 3 Criteria
1) Symptoms and VCS test improve with treatment
2) Lab markers (MMP9, ACTH, etc.) return to normal levels.
So, how do you get diagnosed with CIRS?
In order to make a preliminary diagnosis of CIRS, the clinician must have the following:
- All three of the tier-one criteria
- At least three of the tier-two criteria
Should these two criteria be met, the clinician can proceed with the treatment outlined through the Shoemaker protocol.
Finally, the ultimate confirmation of CIRS occurs if treatment results in an improvement in symptoms, VCS test results, and lab markers.
https://www.survivingmold.com/docs/POA_MOLD_7_27_10_final.pdf
How to be incorrectly diagnosed with CIRS
As CIRS becomes more well known, alternative methods of testing are starting to appear. One type of testing for CIRS that is becoming more common is urinary mycotoxin testing. It is a more readily available test that costs less than the blood work required by the Shoemaker Protocol.
However, this test is very limited and quite often inaccurate when diagnosing CIRS. There are a number of reasons:
-
Lack of Standardization:
There are no regulations guiding urinary mycotoxin testing. As a result, different labs run and interpret urine testing differently. The absence of standardized protocols makes it difficult to establish consistent and reliable results.
-
Questionable Results:
These tests claim to detect mycotoxins produced by molds, but the accuracy of identifying specific mycotoxins and how they relate to clinical symptoms remains uncertain.
-
Inconsistent Excretion Patterns:
Urine is different depending on the hydration levels and kidney function of the patient. It follows that the presence of mycotoxins in urine can be different from patient to patient just depending on how hydrated they are and how well their kidneys work.
-
Metabolite Confusion:
Mycotoxin testing often measures the metabolites of mycotoxins rather than the mycotoxins themselves. The presence of these metabolites can mean many things. It’s quite possible that the test detects metabolites that are present in patients with and without CIRS.
-
Mycotoxin Clearance:
The presence of mycotoxins in urine does not necessarily mean the patient is being exposed to mycotoxins, or that their body can’t clear these toxins. Some individuals may excrete mycotoxins efficiently without developing CIRS symptoms, while others may experience symptoms despite lower mycotoxin levels.
-
Limited Evidence and Clinical Correlation:
There is no solid evidence that shows a direct link between urinary mycotoxin levels and CIRS.
-
Risk of Misdiagnosis:
Just relying on urinary mycotoxin testing for CIRS diagnosis may lead to misdiagnosis and unnecessary (and expensive) treatments. This is because the symptoms of CIRS can overlap with the symptoms of other conditions. A full and proper evaluation by a trained practitioner is important to receive an accurate diagnosis and treatment.
In summary, urinary mycotoxin testing seems to be a straightforward method for assessing mold exposure. However, its limitations and inconsistencies make it an unreliable tool for diagnosing CIRS. The Shoemaker Protocol, developed by Dr. Ritchie Shoemaker, emphasizes a more comprehensive approach that includes a thorough clinical evaluation, specific biomarker testing, and a detailed patient history for a more accurate diagnosis of CIRS.
For a deeper dive into why urinary mycotoxin testing should not be used to diagnose CIRS, check out this paper by Dr. Shoemaker.
The Shoemaker Protocol: A Personalized Path to Healing
The Shoemaker Protocol is a reliable compass guiding individuals through the winding CIRS journey. While many practitioners and websites focus on generalities and making CIRS a one-size-fits-all illness, the Shoemaker Protocol emphasizes the importance of each person’s unique story.
The Shoemaker Protocol incorporates the following pillars:
Empathetic Practitioners:
In the search for a CIRS diagnosis, finding an empathetic practitioner is key. You need a practitioner who listens to your story, acknowledges your struggles, and recognizes that your symptoms are very real. It’s about more than just numbers and results—it’s about the person behind the symptoms.
Flourish Clinic: Navigating the Journey Together
Flourish Clinic understands how complicated chronic fatigue and fibromyalgia are, offers a personalized roadmap through the Shoemaker Protocol. At Flourish Clinic, we understand that each individual’s experience is unique and that true healing requires a holistic approach.
Unraveling Your Unique Story
As you navigate the path to a potential CIRS diagnosis, remember that your story is unique. Beyond routine testing, beyond generic advice, lies your personal path to wellness.
